INTRODUCTION
Urrets-Zavalia syndrome (UZS; fixed dilated pupil) was first recognized by Castroviejo and published in 1963 by Alberto Urrets-Zavalia Jr., who described six cases of atrophic and mydriatic pupil associated with secondary glaucoma following penetrating keratoplasty (PK) in patients with keratoconus(1,2). Other findings of UZS were subsequently reported, including peripheral synechiae, posterior subcapsular opacity, iris ectropion, pigmentary dispersion, and glaukomflecken(3-11).
Other procedures shown to be associated with UZS include trabeculectomy (TREC)(5), deep anterior lamellar keratoplasty (DALK)(12-15), Descemet-stripping automated endothelial keratoplasty (DSAEK)(16-18), cataract surgery(11,19), goniotomy(20), phakic intraocular lens implant (IOL)(21-23), argon laser peripheral iridoplasty (ALPI)(7), and octafluoropropane injection (C3F8)(24).
Although the reported incidence of UZS is low, the associated visual symptoms can cause limitations in activities of daily life requiring preventative measures by ophthalmic surgeons(7,14). The purpose of the present review is to identify all reported cases of UZS published prior to December, 2014 in Medline and EMBASE databases, highlight the most prevalent risk factors, and describe measures for the prevention of Urrets-Zavalia syndrome.
Risk factors and pathogenesis
There are numerous and conflicting risk factors of the development of UZS. Neurogenic changes, inflammatory response, genetic predisposition, and direct iris trauma have all been posited to contribute to the pathophysiology of UZS(7,8,10,25). Early reports indicated the use of atropine in PK as associated with such complications(1). Keratoconus was also suggested to be involved in the pathogenesis of UZS as a result of decreased corneal rigidity and enhanced response to mydriatics(3,26). Intraocular pressure (IOP) elevation, with or without pupillary block, has been implicated as the trigger mechanism of UZS(4,27). Use of viscoelastic substances during surgery have been suspected as toxic to the iris sphincter and a cause of acute rises in IOP(10,11). The use of miotics before and during surgery has been considered prophylactic by some authors and a risk factor of pupillary atrophy by others(4,10,18,25,28).
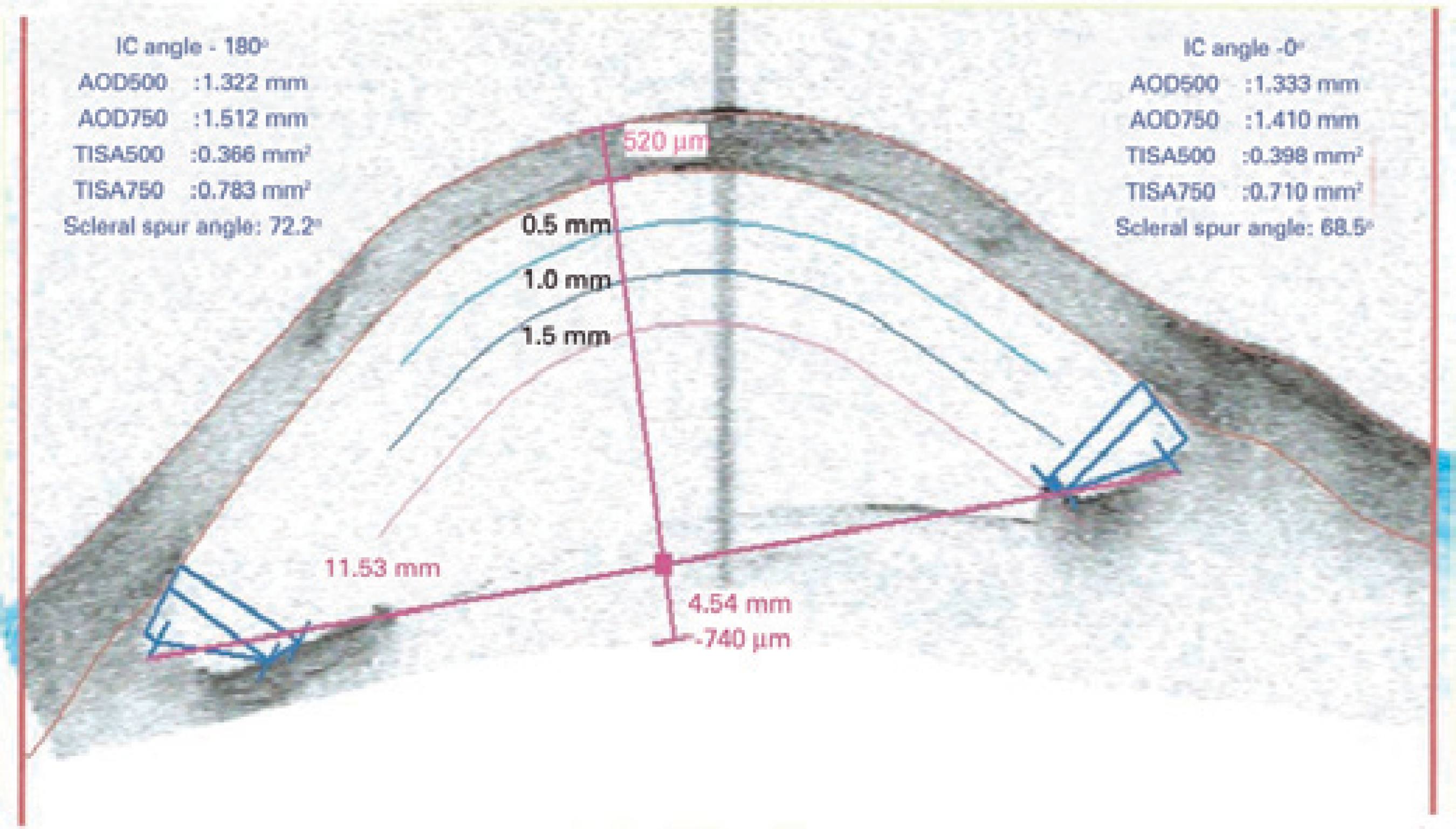
Urrets-Zavalia posited that iris compression against the peripheral cornea under the effect of intense mydriasis without compromising the ciliary body and pars plana was the most important factor related to the development of UZS(1,17). Severe iris ischemia was later reported in several angiography studies(4-6,21). The UZS spectrum comprises anterior segment changes ranging from focal pupillary atrophy with posterior pigment layer injury and no stromal involvement to diffuse or sector atrophy, including the iris stroma(28,29). Ischemic events are not thought to contribute to focal cases and pupillary dilation is considered less intense (6 mm or less). Focal cases of UZS typically respond partially or totally to miotics, which may allow regression of mydriasis. A study on combination therapy with guanethidine and pilocarpine has demonstrated its efficacy and associated miosis in patients with this type of atrophy(28). Conversely, stromal ischemic injury has been reported to be irreversible, promote intense mydriasis (more than 6 mm), and not respond to miotics (Figure 1)(14).
Literature review
More than 30 studies have been published since the first description of UZS, comprising a total of 110 reported cases(1,4-25,29-42). The mean age of the patients in reported cases was 46.1 years (range: 13-90). Reported surgical interventions include PK (51.8%), DALK (18.1%), DSAEK (8.2%), cataract surgery (8.2%), ALPI (8.2%), phakic IOL implantation (2.7%), TREC (1.9%), goniotomy (0.9%), and anterior chamber injection of C3F8 for the treatment of acute hydrops (0.9%). Diagnoses associated with these interventions include keratoconus (45.2%), stromal dystrophies (23.7%), Fuchs' dystrophy (9.4%), plateau iris syndrome (8.5%), senile cataract (8.5%), primary open-angle glaucoma (1.9%), high myopia (1.9%), and congenital glaucoma (0.9%). Individuals affected by bilateral UZS had the same type of ophthalmic procedure on different occasions, corresponding to 8.2% of all patients. The use of mydriatic drops during or after surgical intervention has been reported in only 26% of cases, including the first description of UZS. Viscoelastic was injected to completely maintain the anterior chamber in 44.5% of all surgical procedures. Increased IOP was observed in 59.1% of patients during the first postoperative day and approximately half of these patients (26.7%) had maintained elevated IOP measures during the following days. Only 13.1% of patients with UZS were pseudophakic. Injection of air or C3F8 was performed in 27.3% of cases, particularly in cases of lamellar keratoplasty (89.6% of DALK and DSAEK). The use of miotics (pilocarpine or acetylcholine) was described in 40.9% of patients during the preoperative or intraoperative periods, with 27.3% of patients not receiving any type miotic therapy. There was no reference to the use or not of miotics in 31.8% of the patients.
DISCUSSION
Many retrospective studies and case and series reports of UZS have been published over the past few decades. UZS reportedly has no predilection for age and has been observed as a postoperative response in both young and elderly patients. We believe that the majority of cases of UZS are related to PK, as this has been the predominant technique during the last century(33). In the 1970s, lamellar keratoplasty was used in less than 5% of all transplants(43). With the increasing recognition of lamellar techniques and the use of artificial anterior chambers, reports of UZS increased in subsequent decades. The majority of UZS cases were reported in patients with keratoconus, following the same prevalence pattern as other conditions when considering all uneventful corneal transplantations(29). In a retrospective study that analyzed more than 2,000 patients with PK, the incidence of UZS was higher in patients with macular dystrophy than in patients with keratoconus(7). We believe that patients with keratoconus are not at increased risk of UZS, as stated in previous studies(26). Increased IOP during and immediately after presentation of UZS has been verified in the majority of reported cases; however, the maintenance of ocular hypertension was not clearly demonstrated in these cases(34). This pattern has previously been suggested by some authors(2,5). However, the causal relationship between increased IOP and iris ischemia remains unclear. Progression to secondary glaucoma is reportedly observed in approximately one quarter of cases and should not be considered a definitive characteristic of UZS(2). A retrospective study demonstrated a statistically significant increase in IOP within the first 24 h after surgery in patients undergoing PK for keratoconus(35). Mydriatic instillation during and after the procedure was reportedly performed in a quarter of patients, including the cases originally described by Urrets-Zavalia. Our observations, in corroboration with those of other authors, indicate atropine does not increase the risk of UZS development(32,44-45). In fact, it is questionable whether the use of these measures prevents iris injury(13).
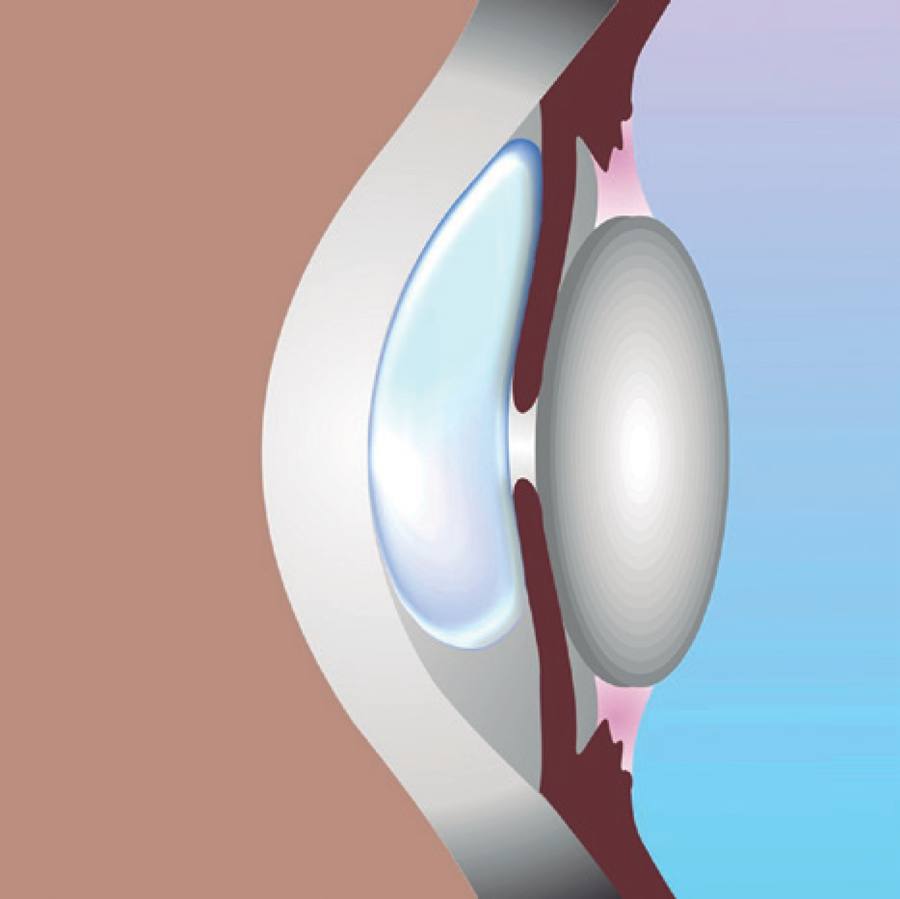
The mechanisms underlying pupillary block remain controversial. It was believed that acute angle closure was required to initiate the pupil atrophy process(5,12,39). Recently, several cases have been described with the absence of pupillary block(10,40). We observed that angle closure was not present in the majority of patients with UZS. The proposed mechanism for iris ischemia in lamellar transplantation is compression against the lens as a result of the injection of large amounts of air or gas into the anterior chamber (Figure 2).
The vast majority of UZS cases are observed in phakic patients. This may explain the limited number of reported cases of UZS in patients undergoing cataract extraction. Protective measures against UZS have also been described, such as iridectomy and intravenous hyperosmotics(8,27). The use of 20% mannitol has been reported to decrease the incidence of UZS from 4% to 1.5%(46). Hyperosmotic agents have demonstrated efficacy in decreasing vitreous volume and subsequently attenuating iris compression due to the lens. Ensuring anterior chamber formation as soon as possible during surgery may also prevent iris strangulation(8). Prophylactic iridectomy or YAG laser iridotomy a few days prior to surgical intervention appear to have efficacy in decreasing risk of pupillary block(2,9,46). However, this practice remains controversial, and some authors have reported that these therapies provide no benefit(11). Careful management of surgical equipment, such as trephines and scissors, may also prevent iris damage(8). There are currently no specific treatments for diffuse pupillary atrophy. Corneal tattooing, specialty contact lenses, and artificial iris implants are options for glare reduction and appearance improvement. In focal atrophy, miotics such as guanethidine and pilocarpine have demonstrated efficacy in treating UZS and attenuating mydriasis(28).
Direct neuronal injury may also be involved in the development of pupillary atrophy. Patients undergoing ALPI may be at risk of damage to the radial parasympathetic fibers of the pupillary constrictor muscle, explaining the observed cases of UZS(7). Likewise, the observation of UZS in both eyes of some patients may indicate a genetic predisposition of the iris sphincter to ischemia in selected corneal pathologies(8). Some authors have attributed the persistence of viscoelastics in the anterior chamber to IOP elevation and UZS. Intraoperative use of viscoelastics was performed in less than half of patients in previous reports. However, the use of viscoelastics is unlikely to be associated with UZS because their use is extremely widespread in cataract extraction surgery and significant pupillary atrophy is not observed following these procedures(47). Despite a lack of data in almost a third of previously reported cases, the use of preoperative and intraoperative miotics was observed in the majority of cases, indicating that these drugs may not prevent irreversible pupil dilation(20,48). Last year, a major review did not address the importance of phakia and the use of miotics in UZS(32).
CONCLUSION
Patient undergoing keratoplasty for the treatment of any corneal pathology, mainly phakic, with increased IOP in the immediate postoperative period and with air or gas left in the anterior chamber are at increased risk of UZS. We believe that the use of viscoelastic or mydriatic substances during or after surgery is not associated with risk of UZS. Pilocarpine and acetylcholine have not demonstrated efficacy in preventing UZS. However, intravenous use of mannitol, IOP control in the immediate postoperative period, and avoidance of massive air or gas injection into the anterior chamber may decrease the incidence of UZS. Iridectomy may be indicated in selected cases, such as patients with increased vitreous pressure, shallow anterior chambers, or the presence of voluminous air or gas in the anterior segment.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

