

Antonio Augusto Velasco e Cruz1; Fernando Chahud2; Rodrigo Feldman1; Patricia Mitiko Santello Akaishi1
DOI: 10.1590/S0004-27492011000100012
ABSTRACT
Posterior scleral tuberculoma formation is an extremely rare condition. The few reports on scleral involvement in tuberculosis refer to cases of anterior scleritis. In the present manuscript we describe a patient who had rheumatoid arthritis and developed a large posterior scleral tuberculoma. The lesion provoked retinal detachment and visual loss and was diagnosed only after enucleation due to a misdiagnosis of choroidal melanoma.
Keywords: Tuberculosis, ocular; Tuberculosis, ocular; Mycobacterium tuberculosis; Sclera; Melanoma; Tuberculoma; Immunosupressive agents; Human; Female; Aged; Case reports
RESUMO
A formação de granuloma tuberculoso na esclera posterior é um evento extremamente raro. Os poucos relatos de acometimento escleral na tuberculose referem-se a casos de esclerite anterior. No presente trabalho é descrito um caso de granuloma escleral posterior em um paciente portador de artrite reumatóide. A lesão provocou descolamento da retina e perda visual e só foi diagnosticada após enucleação por suspeita de melanoma de coróide.
Descritores: Tuberculose ocular; Tuberculose ocular; Mycobacterium tuberculosis; Esclera; Melanoma; Tuberculoma; Imunossupressores; Humano; Feminino; Idoso; Relatos de casos
CASE REPORTS
Posterior scleral tuberculoma: case report
Tuberculoma escleral posterior: relato de caso
Antonio Augusto Velasco e CruzI; Fernando ChahudII; Rodrigo FeldmanI; Patricia Mitiko Santello AkaishiI
IMD, Department of Ophthalmology, Otorhinolaringology and Head and Neck Surgery, Hospital das Clínicas of Ribeirão Preto, São Paulo University, Ribeirão Preto (SP), Brazil
IIMD, Department of Pathology, Hospital das Clínicas of Ribeirão Preto, São Paulo University, Ribeirão Preto (SP), Brazil
ABSTRACT
Posterior scleral tuberculoma formation is an extremely rare condition. The few reports on scleral involvement in tuberculosis refer to cases of anterior scleritis. In the present manuscript we describe a patient who had rheumatoid arthritis and developed a large posterior scleral tuberculoma. The lesion provoked retinal detachment and visual loss and was diagnosed only after enucleation due to a misdiagnosis of choroidal melanoma.
Keywords: Tuberculosis, ocular/diagnosis; Tuberculosis, ocular/immunology; Mycobacterium tuberculosis; Sclera/pathology; Melanoma; Tuberculoma; Immunosupressive agents; Human; Female; Aged; Case reports
RESUMO
A formação de granuloma tuberculoso na esclera posterior é um evento extremamente raro. Os poucos relatos de acometimento escleral na tuberculose referem-se a casos de esclerite anterior. No presente trabalho é descrito um caso de granuloma escleral posterior em um paciente portador de artrite reumatóide. A lesão provocou descolamento da retina e perda visual e só foi diagnosticada após enucleação por suspeita de melanoma de coróide.
Descritores: Tuberculose ocular/diagnóstico; Tuberculose ocular/imunologia; Mycobacterium tuberculosis; Esclera/patologia; Melanoma; Tuberculoma; Imunossupressores; Humano; Feminino; Idoso; Relatos de casos
INTRODUCTION
Tuberculosis (TB) is an ancient illness that remains a global public health problem leading to approximately 1.6 million deaths each year(1). The disease is caused by the Mycobacterium tuberculosis and in rare instances by other members of M. tuberculosis complex such as M. bovis, M. africanum and M. canetti(2). TB can affect any organ or tissue and is typically associated with granuloma formation. In the eye, large lesions (tuberculomas) are usually found only in the choroid(3). In the present report we describe a large posterior scleral tuberculoma that was misdiagnosed as choroidal melanoma. At our best knowledge this is the first well documented case of posterior scleral tuberculosis granuloma.
CASE REPORT
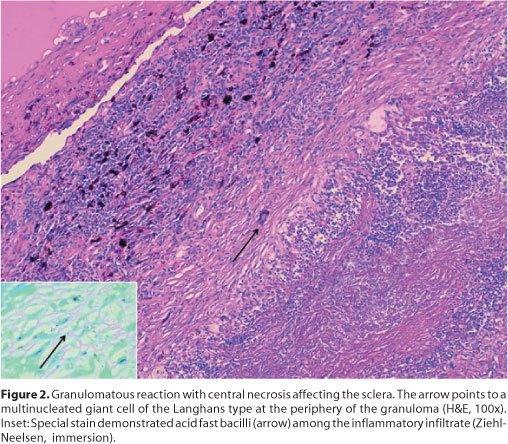
A 66-year-old woman presented with a 3-month history of vision loss in the right eye. The patient was diabetic and had rheumatoid arthritis which had been treated for 8 years with desflazacort (5 mg/day); naproxeno (500 mg/day) and leflunomide (20 mg/day). Purified protein derivative (PPD) test was negative and chest radiograph was normal. The visual acuity was no light perception in OD and 20/30 in OS. Examination of the left eye was unremarkable. In OD there was a dense cataract with 360º posterior synechiae which precluded fundus view. B-scan ultrasonography demonstrated a total retinal detachment overlying a posterior intraocular mass. Topographic and magnetic resonance images revealed that the intraocular mass had no orbital extension. As the findings were compatible with coroidal melanoma, enucleation was advised. After surgery, macroscopic examination disclosed a large (20 x 6 mm) justapapilary scleral nodule (Figure 1). Microscopic examination revealed a granuloma with caseation limited to the sclera. Acid-fast bacilli were found in sections with Ziel-Nielsen staining (Figure 2). A systemic work-up did not show any evidence of tuberculosis elsewhere.
DISCUSSION
It is well known that after the primary pulmonary infection, M. tuberculosis bacilli can spread by lymphohematogenous route and remain dormant inside macrophages over long periods of time. During this latency period the balance between the host immune response and the pathogen can be altered any time in life producing clinical disease in almost every organ of the body (extrapulmonary TB)(2). Granuloma formation is the hallmark of TB. Its function is to contain M. tuberculosis at the site of infection and to prevent dissemination of the pathogen. Morphologically granulomas are formed by a central necrotic core surrounded by layers of macrophages, epithelioid cells, multinucleated Langhans giant cells and lymphocytes(4). The most common clinical presentation of intraocular TB is uveitis(3). In the majority of cases the diagnostic is presumed due to the difficult in microbiological examination(5). Scleral involvement is extremely uncommon. Only a few cases of anterior scleritis have been reported(6). In the eye large granulomas are seen only in the choroid as solitary masses mimicking a tumor(3). We believe that our case is the first well documented large posterior TB scleral granuloma. Different populations of T cells control the granuloma organization(4) and certainly the chronic use of immunosuppressant agents weakened the immune system of our patient provoking the development of such large lesion. The sclera around the optic nerve is perforated by branches of the short ciliary arteries. The rich vascular plexus of this region explains the location of this unique granuloma.
REFERENCES
1. World Health Organization. Global tuberculosis control: surveillance, planning, financing [Internet]. Geneve: WHO; 2007. (WHO/HTM/TB/2007.376). [cited 2010 Jul 27]. Available from: http://www.who.int/tb/publications/global_report/2007/pdf/full.pdf
2. Fitzgerald D, Haas DW. Mycobacterium tuberculosis. In: Mandel GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett's principles and practice of infectious disease. Philadelphia: Elsevier Churchill Livingstone; 2005. p.2852-86.
3. Gupta V, Gupta A, Rao NA. Intraocular tuberculosis - an update. Surv Ophthalmol. 2007; 5(6)2:561-87.
4. Ulrichs T, Kaufmann SH. New insights into the function of granulomas in human tuberculosis. J Pathol. 2006;208(2):261-9.
5. Almeida SR, Finamor LP, Muccioli C. [Ocular manifestation in patients with tuberculosis]. Arq Bras Oftalmol. 2006;69(2):177-9. Portuguese.
6. Saini JS, Sharma A, Pillai P. Scleral tuberculosis. Trop Geogr Med. 1988;40(4):350-2.
 Correspondence address:
Correspondence address:
Patricia Mitiko Santello Akaishi
Hospital das Clínicas - Campus
Av. Bandeirantes, 3.900
Ribeirão Preto (SP) - CEP 14049-900
E-mail: [email protected]
Recebido para publicação em 05.05.2009
Última versão recebida em 30.03.2010
Aprovação em 05.04.2010
Study carried out at the Department of Ophthalmology, Otorhinolaringology and Head and Neck Surgery, Hospital das Clínicas of Ribeirão Preto - USP, Brazil.