

Neşe Alagöz
DOI: 10.5935/0004-2749.20200106
INTRODUCTION
Fusarium species are the commonly encountered agents in cases of fungal keratitis, that develop mostly secondary to trauma or contact lens use(1). Although rare, Fusarium species have been reported to cause endophthalmitis after intraocular surgery(2). The eradication of the fungus is extremely difficult in cases with intraocular involvement, and it requires aggressive treatment with multiple antifungal agents delivered topically, systemically, and intravitreally as well as multiple and repeated surgeries involving keratoplasty, pars plana vitrectomy, lensectomy/intraocular lens removal, and iridectomy. Thus, the final visual outcomes are not typically favorable in patients with fungal endophthalmitis, with up to 60% of eyes eventually being enucleated(1,3).
Improvement in treatment modalities and the early identification of the microorganism has resulted in better management during the acute infectious phase and fewer eyes proceeding to evisceration as compared with the past. However, after eyes are salvaged, they require further management for visual rehabilitation. Herein, we present the longterm followup results of patients involved in a Fusarium endophthalmitis outbreak that occurred in 2008, report the additional surgical procedures that were applied for visual rehabilitation after the acute infectious phase subsided, and discuss the factors influencing the final longterm results.
METHODS
We retrospectively reviewed the medical records of eight patients (three males, five females) who were involved in the fungal endophthalmitis outbreak after cataract surgery performed in the same operating room and on the same date. Although there was variation in surgeons, the common event for all patients was the administration of infused intraocular cefuroximeaxetil from the same vial for all cases. All specimens collected from the patients grew filamentous fungi of Fusarium species.
The study adhered to the tenets of the Declaration of Helsinki, and the local ethical committee approved the study.
RESULTS
Early results regarding the acutephase management and clinical outcomes were previously reported(2). Table 1 summarizes the early and late results. In total, the infection was eradicated in seven eyes, whereas one eye underwent evisceration after corneal involvement and uncontrolled infection (Case 1).
DISCUSSION
Concomitant systemic and ocular diseases seem to be important for the final functional outcome of patients with fungal endophthalmitis. Tissue injury resulting from the acute phase of the disease also appears to influence the longterm outcome.
All patients in our series, except for Case 1, were older than 60 years, and the mean age of the group was 69 years. A previous report defined advanced age as a risk factor for corneal involvement and poor prognosis in Fusarium endophthalmitis(4). The risk factors for Case 1 (eviscerated in acute period) were corneal involvement in the course of the disease and systemic diabetes. Corneal involvement was reported to be the single most important independent predictor of poor final visual outcome in fungal endophthalmitis(5). Case 2, who had unregulated diabetes and diabetic retinopathy, progressed to phthisis during the followup period. In our series, the two patients with surgically managed glaucoma developed graft failure and had a poor final visual outcome, thus pointing out the negative effect of glaucoma on graft survival (Cases 3 and 4).
The only patient who had a good functional outcome did not receive keratoplasty and had no systemic or ocular disease (Figure 1). In our series, this patient had the fewest surgical interventions (Case 6). Typically, a worse longterm outcome was associated with a greater number of surgical interventions (Cases 3 and 4).
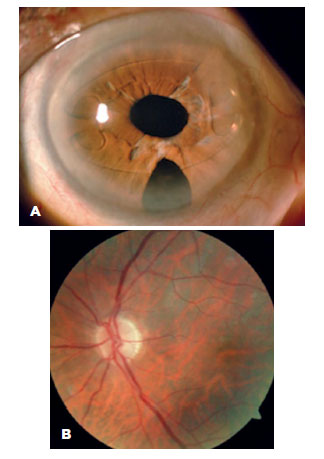
In the eyes in which fundoscopy could be performed during the last examination, paleness of the optic disc was observed to varying degrees. In those patients, advanced age, accompanying systemic diseases, presumed toxicity of the intravitreally administered antifungal drugs, injury from multiple surgeries, and extensive inflammatory reaction in the acute phase all might have contributed to the development of optic neuropathy.
In conclusion, in the treatment of fungal endophthalmitis, successful eradication in the early period was achieved using intensive antifungal therapy and multiple surgical interventions. Despite the additional surgeries performed for visual rehabilitation in our series, only one affected eye maintained useful vision in the longterm.
REFERENCES
1. Dursun D, Fernandez V, Miller D, Alfonso EC. Advanced fusarium keratitis progressing to endophthalmitis. Cornea. 2003;22(4):300-3.
2. Cakir M, Imamoğlu S, Cekiç O, Bozkurt E, Alagöz N, Oksüz L, et al. An outbreak of early-onset endophthalmitis caused by Fusarium species following cataract surgery. Curr Eye Res. 2009; 34(11):988-95.
3. Callanan D, Scott IU, Murray TG, Oxford KW, Bowman CB, Flynn HW Jr. Early onset endophthalmitis caused by Aspergillus species following cataract surgery. Am J Ophthalmol. 2006;142(3):509–11.
4. Güngel H, Eren MH, Pınarcı EY, Altan C, Baylançiçek DO, Kara N, et al. An outbreak of Fusarium solani endophthalmitis after cataract surgery in an eye training and research hospital in Istanbul. Mycoses. 2011;54(6):e767–74.
5. Narang S, Gupta A, Gupta V, Dogra MR, Ram J, Pandav SS, et al. Fungal endophthalmitis following cataract surgery: clinical presentation, microbiological spectrum, and outcome. Am J Ophthalmol. 2001;132(5):609-17.
Submitted for publication:
June 26, 2020.
Accepted for publication:
July 6, 2020.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest:None of the authors have any potential conflicts of interest to disclose.