INTRODUCTION
Herpes simplex keratitis (HSK) is a major cause of vision morbidity worldwide(1,2). Despite improvements in diagnosis and medical treatment, recurrence of HSK is common and leads to severe corneal scarring and sometimes descemetocele formation or perforation. In some cases, corneal transplantation is needed to recover corneal clarity and rehabilitation of visual acuity. Penetrating keratoplasty (PK) is a conventional surgical procedure for treatment of HSK-induced corneal scarring(3-6); however, the success of corneal transplantation due to herpetic corneal scarring is lower as compared to other common indications, such as keratoconus, corneal dystrophy, and bullous keratopathy(7). The reduced survival rate of corneal grafts in patients undergoing PK for herpetic eye disease is mainly attributed to the recurrence of herpetic infection and immune reaction. The postoperative course in these cases can be complicated by high rates of recurrence, graft rejection, and graft failure(8,9).
The purpose of this study was to evaluate the outcome of PK for corneal scarring caused by HSK and to determine whether the type of corneal scar affects the treatment outcome.
METHODS
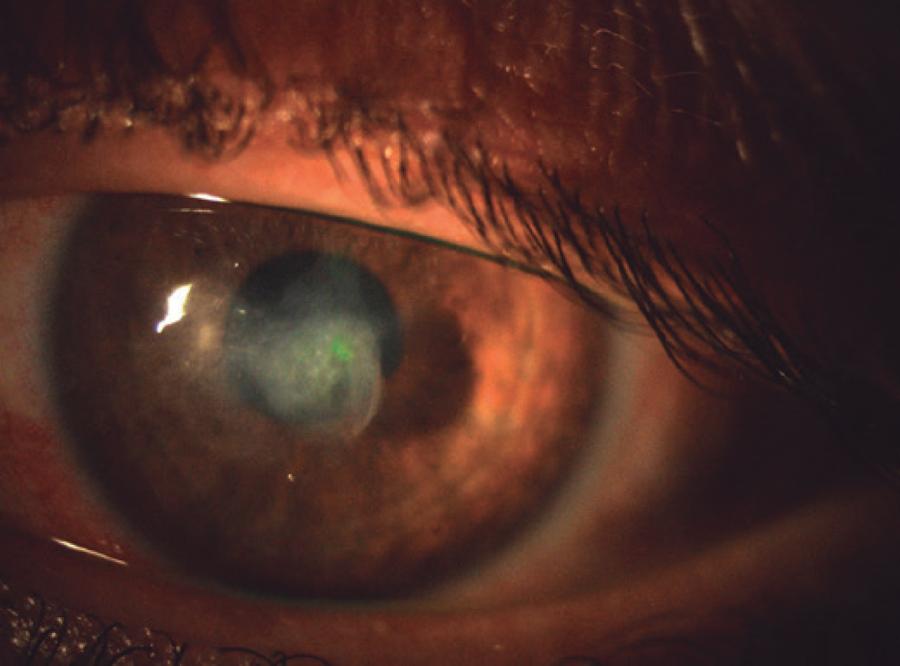
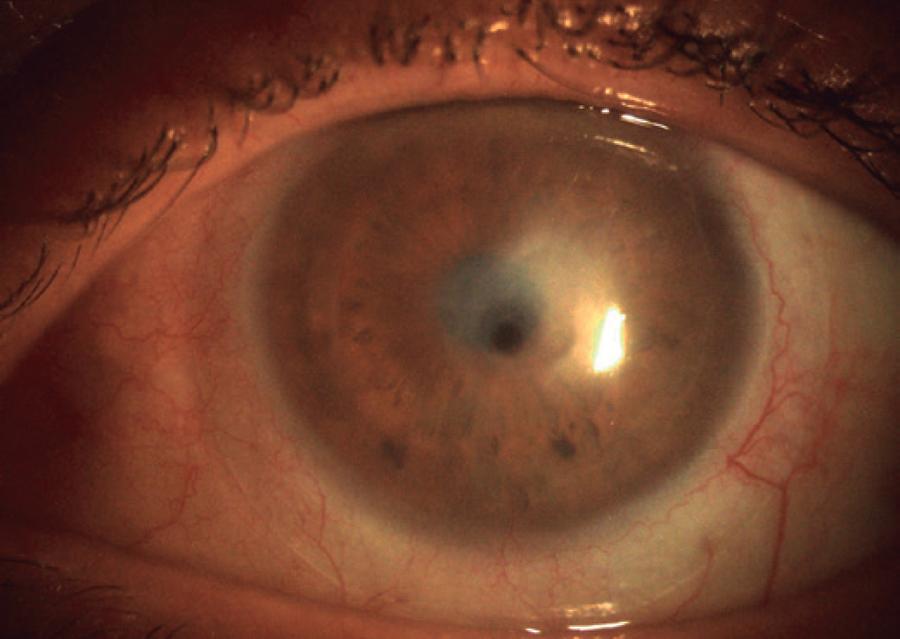
The protocol of this retrospective study was approved by the Ethical Committee of Ankara Training and Research Hospital (Ankara, Turkey) and was conducted in compliance with the tenets of the Declaration of Helsinki. This study enrolled 55 patients with HSK-related corneal scarring who underwent PK (PK) between January 2008 and July 2011, and who had a minimum postoperative follow-up of 18 months. The preoperative diagnosis of herpetic keratitis was based on the history of typical recurrences and clinical manifestations, such as episodes of epithelial dendritic or stromal ulceration with or without inflammatory edema, which responded well to the antiviral therapy. The patients were categorized into two groups. Group 1 consisted of patients who had a quiescent herpetic corneal scar (Figure 1) and group 2 consisted of patients who developed a corneal descemetocele or perforation secondary to persistent epithelial defects with no active stromal inflammation (which was defined as the presence of corneal perforation or descemetocele without typical stromal inflammatory edema of the surrounding cornea in otherwise quiet eyes) (Figure 2).
Preoperatively, the following parameters were recorded for all patients: sex, age, interval without herpetic activation before PK, and best-corrected visual acuity (BCVA). The BCVA of patients was divided into three classifications based on logMAR values: logMAR ≤0.6, logMAR >0.6 to <1.2, and logMAR ≥1.2.
The standard PK procedure was used in all cases. The recipient bed was created by trephination using a trephine of 7.0-7.5 mm in diameter and an oversized fresh button (0.25-0.50 mm) was used for grafting. The recipient-graft junction was fixed with 16 continuous or separate sutures of 10-0 nylon.
Postoperatively, the patients were treated with topical 0.3% ofloxacin and 0.1% dexamethasone sodium phosphate eye drops 6 times daily. Topical steroids were used for 12 months in tapering doses. If intraocular pressure increased, topical antiglaucoma medications were added. All patients received oral acyclovir at 400 mg 5 times daily for the first 3 months, which was tapered to 400 mg twice daily for the following 12 months. Rejection episodes were treated with 0.1% dexamethasone sodium phosphate eye drops every 3 h, which was tapered off over several weeks depending on the clinical response, and the dose of oral acyclovir was adjusted from 200 to 400 mg 5 times daily and then tapered off over 2-3 months. Recurrence of herpes simplex stromal keratitis was treated with oral acyclovir at 400 mg 5 times with 0.1% dexamethasone sodium phosphate eye drops twice daily. In severe cases, daily oral steroid therapy at 40 mg was initiated.
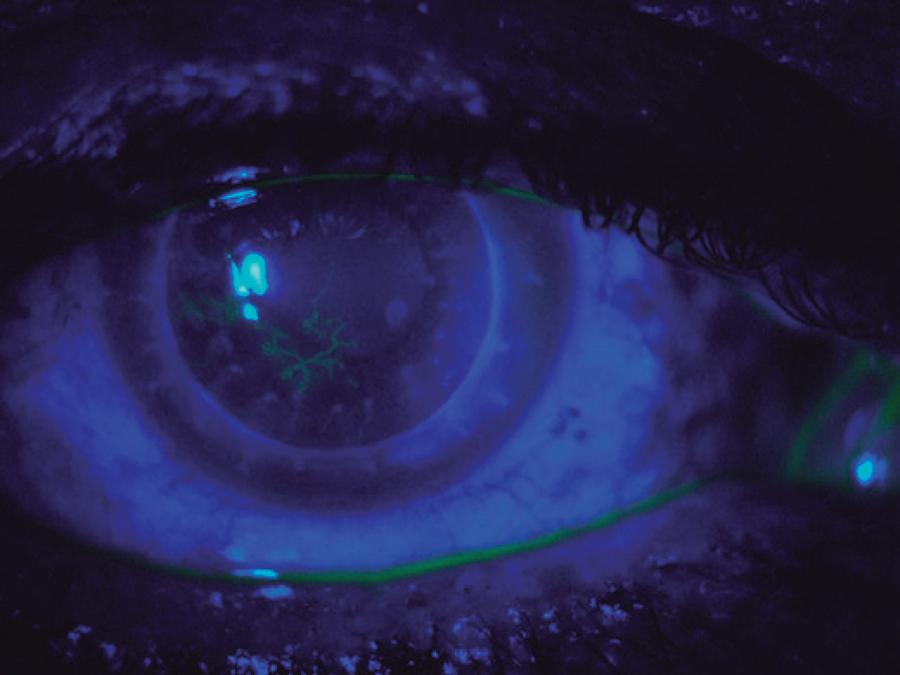
All patients were followed-up at 2 weeks and 1, 3, 6, 12, and 18 months after surgery, and every year thereafter. At each follow-up visit, visual acuity, graft status, and any signs of graft rejection or recurrence of herpetic infection were recorded. Corneal graft rejection was defined as the development of an epithelial or endothelial (Khodadoust) rejection line, spread of corneal edema and keratic precipitates limited to a previously clear graft, and an anterior chamber reaction with decreased vision. Herpetic epithelial recurrence was diagnosed on clinical findings; that is, dendritic or geographic ulceration or a nonhealing epithelial defect. Recurrence of herpetic stromal keratitis was also diagnosed on occurrence of stromal swelling and infiltration, and the presence of keratic precipitates not limited to the graft. Graft failure was defined as irreversible edema and cloudiness of the graft.
Statistical analysis was performed using SPSS software (ver. 15; IBM-SPSS, Inc., Chicago, IL, USA). The effect of the type of herpetic corneal scar on graft survival, graft rejection, and recurrence was investigated using the log-rank test (Mantel-Cox). Kaplan-Meier survival estimates were calculated. The BCVA values at the end of follow-up were compared between the groups using the chi-square test. A probability (p) value of <0.05 was considered statistically significant.
RESULTS
The study enrolled 55 patients, which included 42 patients (9 women/33 men) with a quiescent herpetic corneal scar (group 1) and 13 (2 women/11 men) with a descemetocele or perforated herpetic corneal scar (group 2). The mean patient age was 44.51 ± 14.91 years in group 1 and 41.76 ± 14.33 years in group 2. The mean quiescent period between the last HSV infection and corneal transplantation was 21.77 ± 22.31 months in group 1 and 16.30 ± 20.57 months in group 2. Before surgery, there was no statistically significant difference between the two groups regarding age, sex, and the mean quiescent period between the last HSV infection and corneal transplantation (p=0.56, 0.63, and 0.49, respectively) (Table 1). Preoperative BCVA varied from hand movements to 0.7 logMAR for the entire cohort. Most (93%) of the patients in the herpetic scar group and all (100%) of those in the descemetocele group had a BCVA of ≥1.2 logMAR.
Table 1 Preoperative characteristics of patients and overall survival rates of groups
| Herpetic corneal scar n=42 |
Herpetic corneal scar with perforation n=13 |
Log rank (Mantel-Cox) P |
|
|---|---|---|---|
| Gender | |||
| Male | 33 (78.6%) | 11 (84.6%) | 0.63 (NS) |
| Female | 9 (21.4%) | 2 (15.4%) | |
| Age | 44.51 ± 14.91 | 41.76 ± 14.33 | 0.56 (NS) |
| Mean follow-up | 19.80 ± 12.91 | 26.15 ± 18.85 | 0.17 (NS) |
| Mean inactive duration | 21.77 ± 22.31 | 16.30 ± 20.57 | 0.49 (NS) |
| Recurrence | 12/42 | 4/13 | 0.40 (NS) |
| Recurrence-free survival | 71.4% | 69.2% | |
| Rejection | 4/42 | 3/13 | 0.58 (NS) |
| Rejection-free survival | 90.5% | 76.9% | |
| Graft failure | 8/42 | 4/13 | 0.91 (NS) |
| Graft failure-free survival | 81% | 69.2% |
NS= not significant.
The surgical technique and postoperative management were similar in all patients. The mean donor diameter was 7.50 mm (range, 7.25-8.0 mm). The recipient bed was undersized by 0.25 or 0.50 mm. The mean postoperative follow-up period was 19.80 ± 12.91 months in group 1 and 26.15 ± 18.85 months in group 2 (p=0.17).
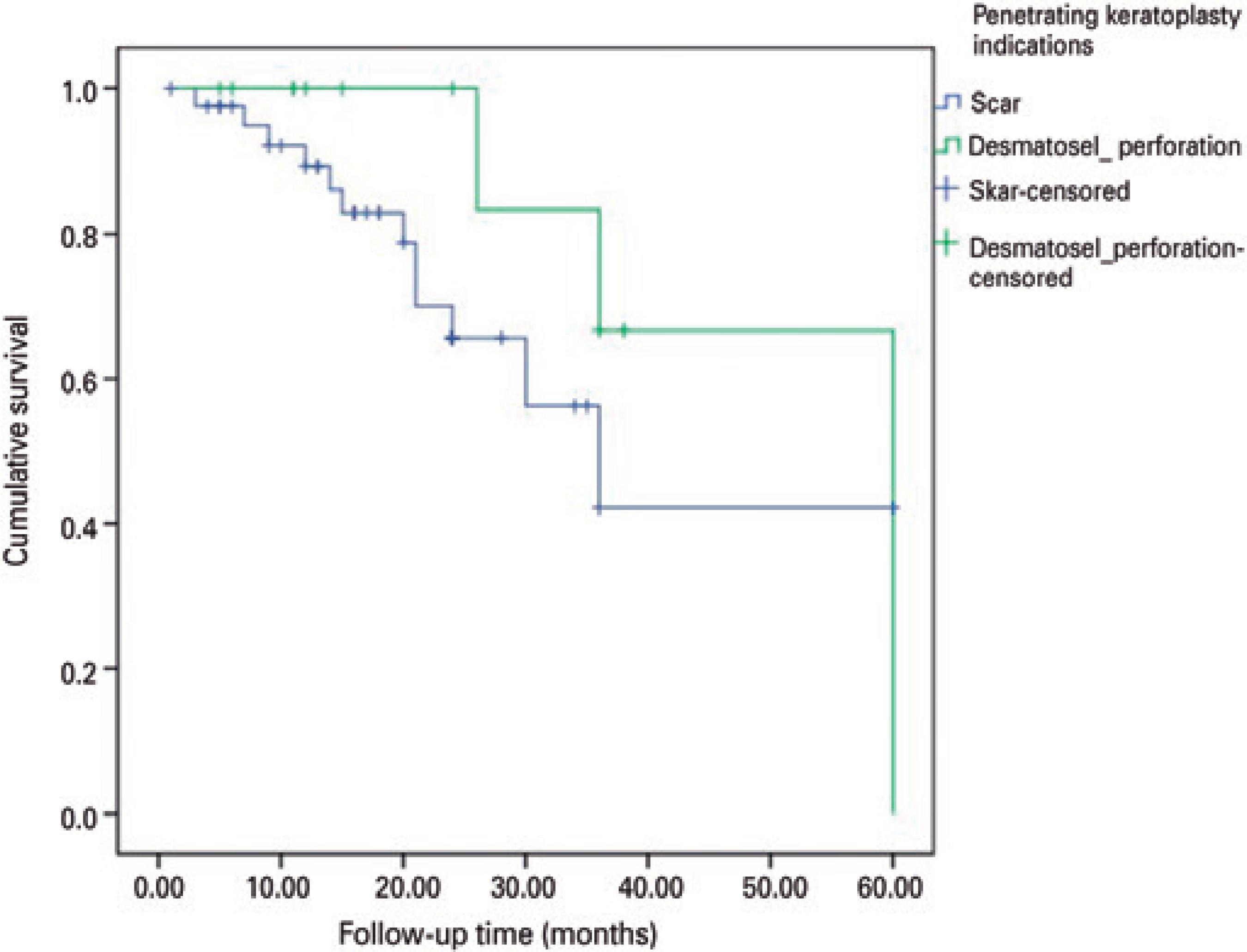
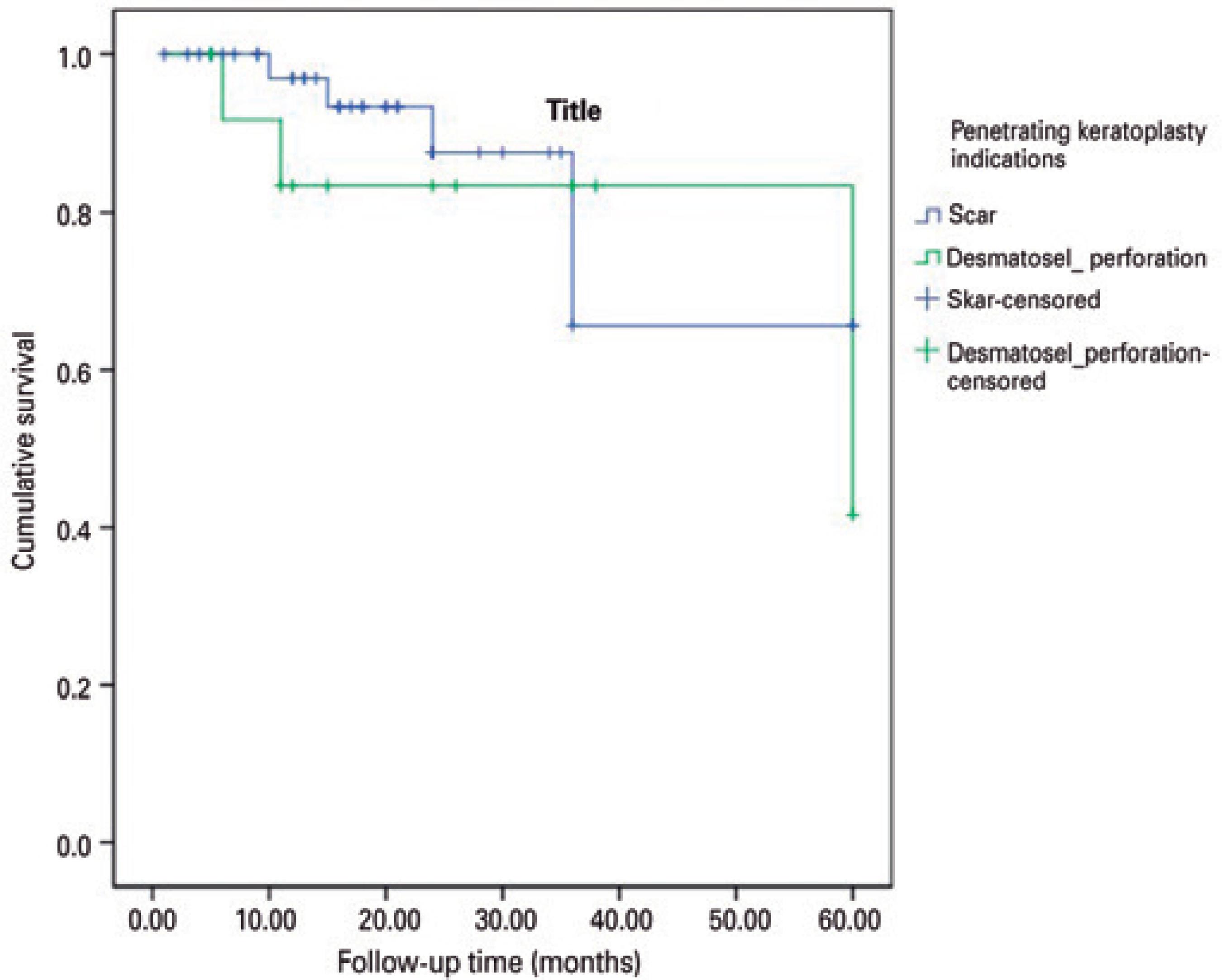
Recurrence of HSV keratitis was found in 12 (28.57%) eyes, which was generally epithelial or epithelial together with stromal keratitis in the quiescent herpetic scar group and the recurrence-free survival rate in this group was 89.3% at 1 year, 65.6% at 2 years, and 42% at 3 years (Figure 3). When limited to 13 patients with a herpetic corneal scar with a descemetocele or perforation, recurrence was found in 4 (30.76%) eyes and recurrence-free survival in this group was 100% at 1 year, 83.3% at 2 years, and 63.6% at 3 years. The difference between groups was not statistically significant (p=0.40) (Figure 4) (Table 1).
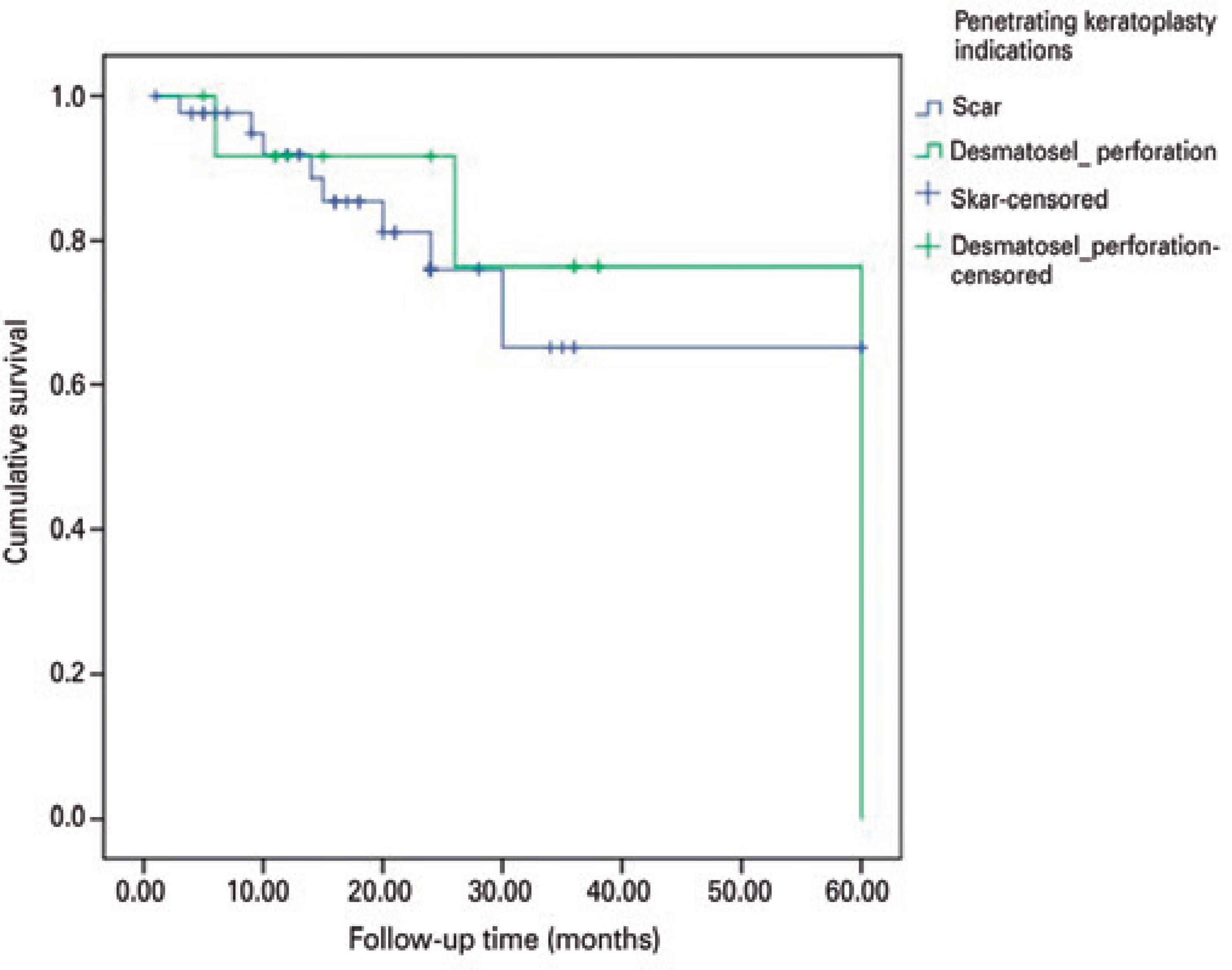
Graft rejection occurred in 4 eyes of 42 patients (9.52%) in group 1 (including the 2 eyes with recurrent HSV keratitis) and the rejection-free survival was 97% at 1 year, 87.5% at 2 years, and 65.7% at 3 years. In group 2, graft rejection occurred in 3 eyes of 13 (23.07%) patients and the rejection-free survival was 83.3% at 1 year, 76.4% at 2 years, and 63.6% at 3 years. The difference between groups was not statistically significant (p=0.58). All rejections in both groups were the endothelial rejection type (Figure 5).
Graft failure occurred in 8 (19.04%) eyes at a mean duration of 24.5 months (range 8-60 months) in group 1, among which the causes for graft failure included rejection in 2 patients and recurrence of HSV keratitis in 6 patients. In group 1, the graft survival rate was 91.9% at 1 year, 76.0% at 2 years, and 65.1% at 3 years. In group 2, graft failure developed in 4 of 13 eyes (30.76%) and the graft survival rate was 89.5% at 1 year, 76.0% at 2 years, and 63.6% at 3 years. The difference between groups was not statistically significant (p=0.91) (Figure 6).
Of the entire cohort, 34 (61.8%) patients achieved visual acuity of 0.6 logMAR or better, whereas 11 eyes (20%) had a postoperative BCVA worse than 1.2 logMAR because of graft rejection or failure. At the end of the follow-up, 28 (66.7%) patients in the herpetic corneal scar group and 6 (46.2%) in the descemetocele group had a BCVA of <0.6 logMAR, 7 (16.7%) patients in the scar group and 3 (23.1%) in the descemetocele group had a BCVA between 0.6 and 1.2 logMAR, and 7 (16.7%) patients in the scar group and 4 (30.8%) in the descemetocele group had a BCVA of >1.2 logMAR. There were no statistically significant differences between groups (p=0.38, chi-square test).
DISCUSSION
In this study, the long-term outcomes of PK for treatment of HSKinduced corneal scarring are reported. In general, corneal surgeons hesitate to perform corneal transplantation for the management of herpetic corneal disease because the long-term success is relatively poor due to immunologic graft failure. HSK can also recur in corneal allografts and is sometimes difficult to distinguish from graft rejection. Recurrent HSV infection usually follows reactivation of latent virus in the trigeminal ganglion, although the use of corticosteroids after PK may be a triggering factor(10,11). Due to inflammation, recurrence of HSK after PK is associated with an increased risk of graft rejection. In addition, in the case of combined HSK recurrence and graft rejection, drug application is more difficult(4). The use of oral antivirals for prophylaxis can significantly reduce the recurrence rate of herpes. Nonetheless, these grafts remain at a higher risk for failure from immunologic rejection. Acyclovir, an acyclic purine nucleoside analog, is the most commonly used antiviral medication(12-15).
In this study, recurrence of epithelial keratitis or epithelial together with stromal keratitis was the major type of recurrence of HSV keratitis, similar to that reported in previous studies(16,17). The recurrence rate was 28.57% in group 1 and 30.76% in group 2, but this difference was not statistically significant (p=0.40). Several studies have reported different recurrence rates of HSV keratitis after PK(12,16,18). For example, Wu et al. reported a recurrence rate of 20.6% after PK for herpetic corneal scarring and 1-, 2-, and 3-year recurrence-free survival rates of 88.9%, 85.1%, and 77.9%, respectively(16); however, this study did not enroll patients with HSK-induced corneal leucoma with a history of corneal perforation and the patients received oral acyclovir at 200 mg 5 times daily for the first 3 months, which was then tapered to 400 mg twice daily for a further 12-18 months(17). Awan et al. reported recurrence of herpetic corneal scarring in 33% of 18 patients following deep anterior lamellar keratoplasty and oral acyclovir at 200 mg twice daily for 12 months. In that study, the mean preoperative disease-free duration was 2 years(18). The difference in recurrence rates and recurrence-free survival between those studies can be mainly attributed to preoperative disease-free duration and use of prophylactic antiviral therapy.
In the present study, the rejection rate was 9.52% in the quiescent herpetic scar group and 23.07% in the descemetocele or perforated herpetic scar group. Rejection-free survival rates at 1, 2, and 3 years were 97.0%, 87.5% and 65.7% in group 1, and 83.3%, 76.4% and 63.6% in group 2, respectively. Although the rejection rates seemed higher in group 1 than in group 2, rejection-free survival was similar at 3 years between groups (p=0.58). Garcia et al. reported 1-, 2-, and 3-year rejection-free survival rates of 83.6%, 77.2%, and 74.5%, respectively, in those patients who received oral 400 mg acyclovir twice daily(15). They measured host vascularity by the number of involved quadrants and found no association with allograft rejection or failure. The rejection-free survival rates at 1 and 2 years in group 1 of this study were higher than those reported by Garcia et al., which may have resulted from the dose and duration of oral acyclovir treatment; however, the rejection rate in group 2 in this study was higher than in group 1, which can be attributed to perforation-induced corneal inflammation and/or to the small number of subjects in group 2. This study has some shortcomings: 1) it is a retrospective study, and 2) host vascularity was not recorded preoperatively.
A total of 8 grafts (19.04%) failed in group 1, one half due to graft rejection and the other half due to recurrence. When limited to only 13 patients in group 2, 4 (30.76%) grafts failed. The failure rate of group 1 was markedly lower than that in the study by Moyes et al.(17), where the failure rate was 30%. A possible explanation for this difference is the routine use of prophylactic oral acyclovir in our patients, as several other studies reported lower graft failure rates with the routine use of prophylactic oral acyclovir(4,19). Another possibility is that the mean preoperative disease-free duration in the present study was 21.77 ± 22.31 months in group 1 and 16.30 ± 20.57 months in group 2. Unfortunately, these data were not available for comparison for the cohort of Moyes et al.; however, Garcia et al. reported a failure rate of 11.4% with a 56-month disease-free duration before surgery, which could have led to better postoperative graft survival(15).
In this study, although the recurrence and graft rejection rates differed between the two groups, the 3-year graft survival rates were similar (65.7% and 63.6%, respectively). In a study by Killingsworth et al., 15 patients who required therapeutic PK for HSK were divided into two groups. The first group included patients with severe stromal keratitis who did not respond to medical treatment and patients who progressed to perforation. The second group consisted of patients who developed corneal perforation without active inflammation. Only 4 of the 11 patients in the first group achieved clear grafts, whereas all 4 patients in the second group achieved clear grafts(20). Likewise, according to our results, without inflammation, corneal herpetic scarring with a descemetocele or perforation, achieved close graft survival and quiescence of the herpetic corneal scar.
CONCLUSION
It has already been reported that corneal grafts had a significantly high risk of rejection and failure in cases with underlying herpetic disease. Epstein et al. and Gittins-Nunez et al. found that the incidence of graft failure after rejection episodes was significantly greater in grafts for herpes, as compared to grafts for keratoconus(21,22). In this study, without inflammation, cases with corneal herpetic scarring with a descemetocele or perforation achieved similar graft survival rates with quiescent herpetic corneal scarring. The preoperative disease-free interval and dose and duration of prophylactic systemic acyclovir therapy are major factors affecting the graft survival.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

