INTRODUCTION
Pregnancy is associated with metabolic, hormonal, and hemodynamic changes. The renin-angiotensin system regulates salt and water hemostasis in the body, and both renin and angiotensin levels increase during pregnancy. These changes lead to increasing blood volume beginning in the first trimester( 1 , 2 ). Systemic vascular resistance decreases during pregnancy( 3 , 4 ), and hemodynamic changes affect blood pressure. In normal pregnancy, blood pressure initially decreases until the eighteenth to twentieth gestation week, but then increases until delivery( 5 , 6 ). One study reported that total macular volume and foveal retinal thickness increase during pregnancy in the second and third trimesters because of fluid accumulation( 7 ). During pregnancy, hemodynamic changes affect other parts of the body, including choroidal flow.
The choroid is the vascular layer between the retina and the sclera that provides the blood supply to the eye and plays an important role in ocular nutrition. Histopathological examination showed that it is 0.22 mm thick posteriorly( 8 ). The choroid is composed of a vascular network that contributes to ocular nutrition through volume regulation and is extremely sensitive to blood pressure changes. The choroidal thickness is affected by blood flow and perfusion pressure( 9 ). Therefore, hemodynamic alterations can affect choroidal thickness.
Optical coherence tomography (OCT) provides high-resolution, cross-sectional digital images of live biological tissues in vivo. With the use of enhanced depth imaging optical coherence tomography (EDI-OCT), choroid images can be obtained and the choroidal thickness can be measured. Using OCT, one study reported the choroid thickness as 287 µm, 261 µm, and 145 µm at subfoveal regions, 3 mm temporal to the fovea, and 3 mm nasal to the fovea, respectively, in healthy individuals( 10 ). The change in the choroid thickness may play a role in the pathophysiology of various ocular conditions.
In the present study, we used EDI-OCT to examine choroidal thickness at each trimester in healthy pregnant women, and then compared these measures with those for non-pregnant healthy women.
METHODS
We examined 4 groups in the present study. Group 1 consisted of 30 eyes in 30 healthy women in the first trimester, group 2 consisted of 30 eyes in 30 healthy women in the second trimester, and group 3 consisted of 30 eyes of 30 healthy women in the third trimester. Group 4 was the control group and consisted of 30 eyes in 30 healthy non-pregnant women. Only the right eye was assessed in each study participant. This study followed the tenets of the Declaration of Helsinki. All participants provided informed consent. The inclusion criteria for groups 1, 2, and 3 were healthy pregnant women in their first, second, or third trimester Inclusion criteria for the control group (group 4) included an age of 18-40 years old, non-pregnant healthy regularly menstruating women. High myopic and hyperopic refractive errors greater than -1.0 or +1.0 diopters, or intraocular surgical intervention were excluded from the study. Subjects with systemic diseases or conditions that might affect retinal or choroidal thickness were excluded. For example, patients with diabetes mellitus were excluded. Pregnant with high blood pressure was excluded. In addition, patients with any retinal or choroidal abnormalities detected in spectral-domain OCT scans were excluded.
All subjects underwent a thorough ocular examination, including an auto-refractometer, best-corrected visual acuity measurement, slit-lamp examination, intraocular pressure measurement, and dilated funduscopy. Choroidal thickness was measured using a spectraldomain OCT device (Spectralis: wavelength, 870 nm; Heidelberg Engineering, Germany) with an enhanced depth-imaging mode after pupil dilation. All measurements were performed in the morning. The horizontal section running through the center of the fovea was selected for further analysis. The OCT images were assessed independently by 2 ophthalmologists.
The choroidal thickness was measured from the outer portion of the hyperreflective line, corresponding to the retinal pigment epithelium, to the inner surface of the sclera. Choroidal thickness was measured at the fovea and at positions 3 mm temporal, and nasal to the fovea. The values of the measurements were compared for each observer and then averaged for analysis.
Diastolic blood pressure, systolic blood pressure, and ocular perfusion pressure were measured for each subject. Ocular perfusion pressure was calculated according to the following formula( 11 ): Ocular perfusion pressure = mean blood pressure - intraocular pressure.
Statistical calculations were performed using SPSS (Statistical Package for Social Sciences version 15.0; SPSS, Inc., Chicago, IL). Choroidal thickness is presented as the mean ± standard deviation. The Kolmogorov-Smirnov test was used to assess correlations for data with a normal distribution. Groups were compared with an analysis of variance (ANOVA) and post hoc tests. The differences in choroidal thickness detected by ANOVA and post hoc tests between healthy (control group) and pregnant individuals were also analyzed by the t-test. P values less than 0.05 were considered significant.
RESULTS
Ninety eyes in 90 healthy pregnant women and 30 eyes of 30 age-matched healthy non-pregnant women were included. The mean gestational age was 7.4 ± 2.6, 19.2 ± 2.9, and 33.1 ± 2.8 weeks in groups 1, 2, and 3, respectively. Mean age was 28.5 ± 6.4, 26.6 ± 4.2, 26.9 ± 6.2, and 29.4 ± .2 years, in groups 1, 2, 3, and 4, respectively. There were no statistically significant differences in age among the groups (p=0.183). Representative EDI-OCT scans for a pregnant women and the control group is presented in figure 1. Table 1 shows the mean choroidal thickness values for the groups that were measured at subfoveal regions, and those 3 mm nasal to fovea, and 3 mm temporal to fovea. There were statistically significant differences in subfoveal, temporal, and nasal choroidal thickness among the groups (p<0.05). The mean subfoveal, temporal, and nasal choroidal thickness was significantly greater in group 2 compared with the control group (p=0.007, p<0.001, p=0.026, respectively). There was no difference in mean subfoveal, nasal, and temporal choroidal thickness between group 1 and the control group (p=0.214, p=0.177, p=0.094, respectively). There was also no statistical significance among the 3 groups and control group for the mean subfoveal, temporal, and nasal choroidal thickness (p=0.105, p=0.261, p=0.695, respectively). Figure 2 shows the distribution of choroidal thickness according to group.
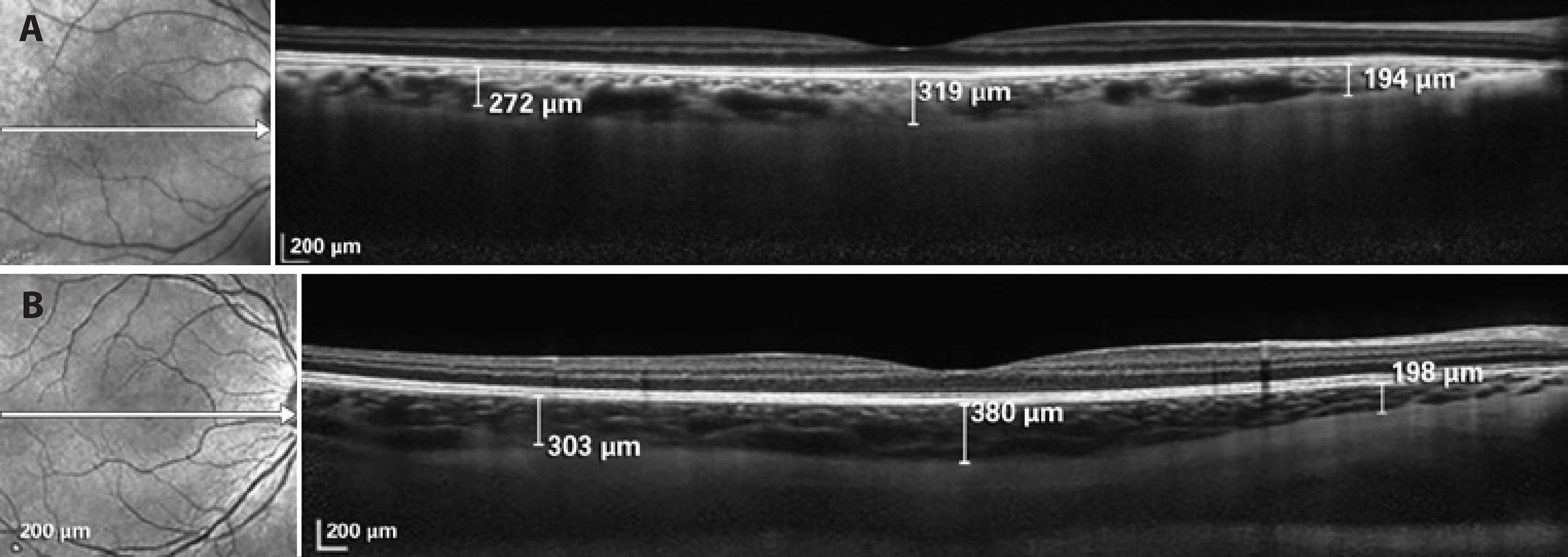
Figure 1 A) Optical coherence tomography image from the control group demonstrating enhanced depth imaging on Spectralis (Heidelberg Engineering). The choroidal thickness was measured from the outer portion of the hyperreflective line, corresponding to the retinal pigment epithelium to the inner surface of the sclera at the subfovea, 3 mm temporal, and 3 mm nasal to the fovea. Calipers were positioned manually using computer software provided by the manufacturer. B) Optical coherence tomography image from second trimester, which depicts the increased the choroidal thickness.
Table 1 Mean choroidal thickness values (μm) for each group
| Location | Group 1 (n=30) | Group 2 (n=30) | Group 3 (n=30) | Group 4 (n=30) | P* control |
|---|---|---|---|---|---|
| first trimester | second trimester | third trimester | |||
| Subfoveal | 362 ± 81 | 395 ± 80 | 368 ± 70 | 335 ± 86 | 0.037 |
| Temporal | 297 ± 73 | 338 ± 74 | 293 ± 72 | 274 ± 54 | 0.004 |
| Nasal | 225 ± 60 | 233 ± 61 | 205 ± 46 | 200 ± 53 | 0.044 |
Values are presented as the mean ± SD.
*= ANOVA test
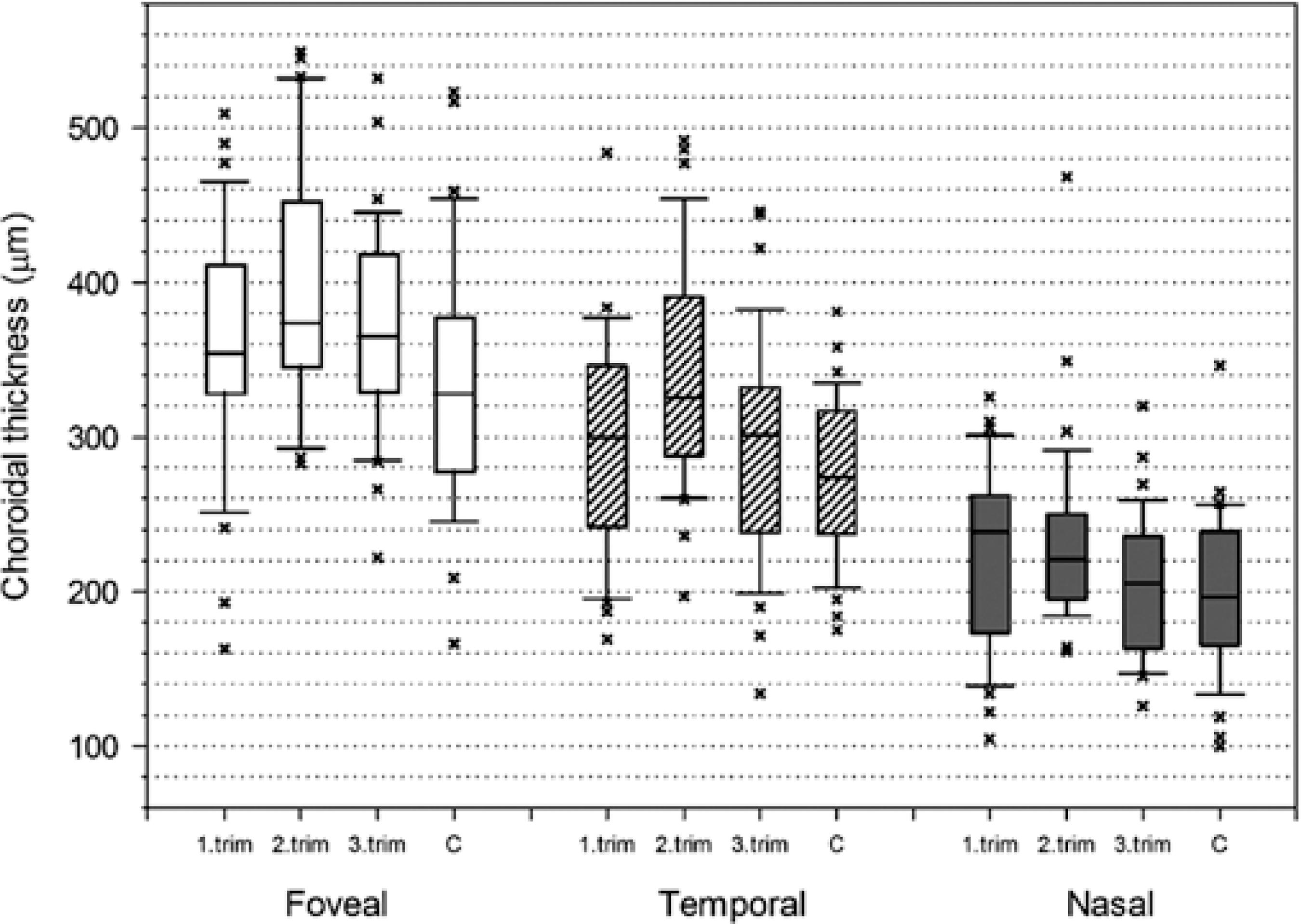
Figure 2 Graph showing subfoveal, temporal, and nasal choroidal thickness distribution according to groups.
The ocular perfusion pressure was 36.3 ± 3.5 mmHg in pregnant women and 37.3 ± 2.8 mmHg in the control group. No significant correlations were found between the choroidal thickness and ocular perfusion pressure, gestational week.
DISCUSSION
Pregnancy can affect the eyes. Non-pathological events occurring during pregnancy includes reduced corneal sensitivity and increased corneal thickness related to the water retention. Choroidal thickness changes can be expected because of this water retention. There are some additional pathologic conditions reported to develop during pregnancy such as central serous chorioretinopathy( 12 ). However, few studies have investigated choroid thickness in pregnant women( 13 - 15 ). Takahashi et al. have demonstrated that there was no significant difference in choroidal thickness between healthy pregnant and non-pregnant women at the subfoveal and other measurement points( 13 ). However, only the pregnant women in the third trimester were included in that study. Similarly, we did not find any difference in choroidal thickness measurement between pregnant women in the third trimester and the control group. Kara et al. investigated pregnant women in 15-38 weeks of gestational age( 14 ). They reported that subfoveal choroidal thickness increased in pregnant women but no significant correlation between the choroidal thickness and gestational age was found. Sayin et al. investigated pregnant women in 17-37 weeks of gestational age( 15 ). They reported that subfoveal choroidal thickness increased in pregnant women and found that negative correlation between the choroidal thickness and gestational age. As distinct from these studies, we examined the mean choroidal thickness in pregnant subjects in each trimester via EDI-OCT. To our knowledge, the current study is the first to investigate the choroidal thickness in three trimesters compared with non-pregnant healthy women. It can be considered as an important finding that the choroidal thickness significantly increased in the second trimester but it did not change in the first and third trimesters.
While blood volume progressively increases, a rapid increase is typically noted until mid-pregnancy, with a slower increase thereafter. Additionally, during pregnancy, vascular resistance decreases from the fifth week of the gestation due to hormonal change( 3 , 4 ). As vascular resistance decreases, vascular compliance increases( 16 ). The decrease of the vascular resistance results in reduced blood pressure particularly in the mid-pregnancy. Thereafter, systemic pressure begins to increase again and ultimately reaches or exceeds the pre-pregnancy level( 17 ). The reduction of blood pressure and systemic vascular resistance, which is observed particularly in the middle of pregnancy, may explain the increase in choroidal thickness in the second trimester.
During pregnancy blood flow increases in many organs, including the kidneys, extremities, and skin( 18 - 20 ). One study reported increased ocular blood flow during pregnancy caused by vasodilation due to estrogen change( 21 ). We suggest that increased choroidal thickness may be secondary to increased blood flow.
Choroidal changes during pregnancy may play a vital role in the pathophysiology of ocular diseases such as central serous chorioretinopathy. Choroidal vasodilation and choroidal vascular hyperpermeability causes subsequent vascular leakage resulting in increased hydrostatic pressure in the choroid. Recent studies demonstrated a significantly increased choroidal thickness in patients with acute central serous chorioretinopathy( 22 , 23 ). Central serous chorioretinopathy may be caused by an increased hydrostatic pressure in the choroid. Pregnancy is one of the several known risk factors for central serous chorioretinopathy, which commonly develops in the third trimester( 24 ). We speculate the increased choroidal thickness observed in the second trimester may be the causative factor underlying development of central serous chorioretinopathy in the third trimester. This may explain why central serous chorioretinopathy is more commonly observed in the third trimester.
The current study has several limitations. First, we did not measure ocular blood flow. Color Doppler imaging can measure the velocity of blood and vascular resistance within each vessel( 25 ). Although this technique is useful for determining choroidal blood flow, it does not provide three-dimensional anatomical information about the choroidal layers. In our study, ocular blood flow was not examined; therefore, our study cannot determine the relationship between choroidal thickness and ocular blood flow. We can speculate that the thicker choroid may indicate an overall increase in choroidal blood flow in pregnant women, as was previously demonstrated with a pulsatile ocular blood flow pneumotonometer( 21 ). Therefore, it is likely that the increased choroidal thickness may be related to increased ocular blood flow. Another limitation of our study was the small number of participants.
High refraction and age affect the thickness of the choroid( 10 , 26 ). Consequently, in our study we included similar groups with respect to meaningful characteristics, such as age and refraction, for both the pregnant and control groups.
In conclusion, our study showed a significant increase in choroidal thickness in the second trimester whereas there was no increase in the choroidal thickness during the first and third trimesters. These data favor the idea that in pregnant women, increased choroidal thickness may lead to increased vascular permeability, which can explain the relationship between pregnancy and central serous chorioretinopathy. Further studies with a larger number of subjects should be performed in a pregnant population to correlate choroidal blood flow with choroidal thickness.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

